Neuropathology is a histology specialty unto itself. Most hospitals and healthcare facilities will refer patients to a neuropathology center. Specimens can be procured by neurosurgery (i.e. tumor samples, brain biopsies, peripheral nerve biopsies, skeletal muscle biopsy) or post mortem (i.e. whole brain or spinal cord).
While your laboratory may not receive neuropathology specimens, there may be times when you might be consulted regarding fixation and processing of such specimens. Brain and spinal cord biopsies are tiny in nature, and the specimens are usually “sticky”. Parafilm or a piece of polythene, folded over to prevent drying, may be used to receive and transport fresh specimens. These may subsequently be frozen for rapid frozen section diagnosis.
Alternatively, 10% neutral buffered formalin may be used as a fixative for routine processing of larger tissue samples (i.e. post mortem specimens) into paraffin blocks. Subsequent processing protocols employ long processing times, to facilitate complete dehydration and infiltration of paraffin into the myelin.
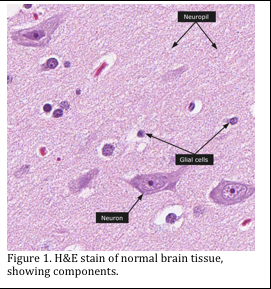
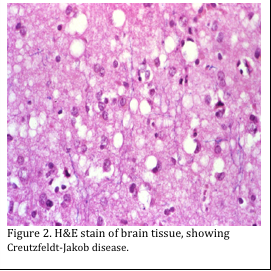
It is important to note that brain, spinal and nerve tissue may contain transmissible spongiform encephalopathies (TSE) or prion diseases, which are neurodegenerative diseases that can affect humans and a variety of domestic and wild animal species. Prions are the causative agent of Creutzfeldt-Jakob disease in humans. The resulting holes in the brain tissue are remarkable (Figure 1 and 2). These infective prion agents are not inactivated by 10% formalin, so they remain potentially infectious, even after routine processing into paraffin. Formalin-fixed and paraffin-embedded tissues, especially of the brain, remain infectious. Treatment of formalin-fixed tissues from suspected cases for 30 min in 96% formic acid or phenol before histopathologic processing is considered to inactivate the prions, but such treatment may severely distort the microscopic neuropathology (Ref 4).
The safest method for ensuring that there is no risk of residual infectivity on contaminated instruments and other materials is to discard and destroy them by incineration.
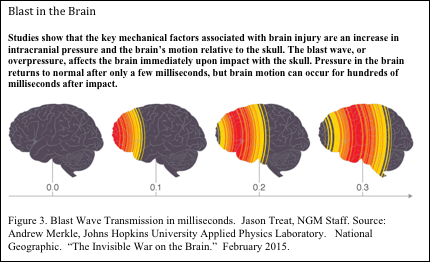
The following is taken from two references: (1) National Geographic, “The Invisible War on the Brain.” February 2015, and (2) the “Neurologic Rehabilitation Institute at Brookhaven Hospital’ website.
“Military Brain Injury Study (Brookhaven Institute) Taking a play from the playbook of the National Football League, the US Military has created a “Brain Bank” repository program for the study of Traumatic Brain Injury (TBI) in veterans called the Center for Neuroscience and Regenerative Medicine Brain Tissue Repository for Traumatic Brain Injury. The donations are entirely voluntary and the study is not allowed to approach family members of the deceased to request donations to the study.
Since the launching of the study launched in June of 2013, the program has received numerous requests for information along with brain donations. The lab is attempting to collect several hundred brains from soldiers with and without a history of TBI. The goal of the research is to study the sections of the brain that are most susceptible to damage, as well as possible symptoms related to those damaged areas.
Per a recent article in Forbes magazine, Dr. Daniel Perl, the director of the repository cautioned “against the impulse to lump soldiers and football players together before the repository research is completed. Football players may bash their heads on a regular basis, but they aren’t exposed to explosions. “It’s important for us to not just say, ‘Okay he’s got tau, he’s like a football player.’”
Discovery of the similarities and differences between combat trauma injuries and those found in the NFL studies could prove to be very interesting.
References:
- National Geographic. “The Invisible War on the Brain.” February 2015.
- Neurologic Rehabilitation Institute at Brookhaven Hospital
- http://www.traumaticbraininjury.net/military-brain-injury-study/
- www.cdc.org


