Fungi include molds, yeasts and higher fungi. All fungi are eukaryotic and have sterols but not peptidoglycan in their cell membrane. Their cell walls are composed of cellulose; the same building blocks that plants use. Fungi may produce large, reproductive mycelium, called mushrooms, which may be edible, or poisonous. Other naturally occurring fungi may infect humans, one example being “athlete’s foot”.
Fungi are chemoheterotrophs which require organic nutrition and most are aerobic. Many fungi are also saprophytes which live off of dead organic matter, in soil and water and acquire their food by absorption. Fungi may produce sexual and asexual spores. There are over 100,000 species recognized, with over 100 of them known to be infectious agents in humans. Molds are composed of numerous, microscopic, branching hyphae known collectively as a mycelium.
Hyphae growth occurs from the apical tip, and apical vesicles contain materials and enzymes for the formation of new hyphal wall. Older hyphae are less biochemically active and contain many storage vacuoles. In most molds these hyphae have septa, which are cross-walled divisions, but in some there are none and the hyphae are aseptate. A septum is a cross-wall formation which divides one fungal hypha into two cells. These septa may add strength to the hyphae or serve to isolate adjacent parts to allow differentiation, such as during production of the reproductive structures.
Pure white slides for special staining and IHC
Specially designed with an aggressive adhesive coating for the toughest staining routines. The Rankin Basics IHC slides are made of pure white glass, which prevents auto-florescence. Each case is vacuum sealed and specially coated to prevent sticking. Request your free sample today.

Rankin Basics IHC Microscope Slides, Pure White, Extra Adhesion – Case/1,440
Spores are formed from the reproductive mycelium. Asexual spores are produced by the aerial mycelium of a single organism, whereas sexual spores are formed by the fusion of cells and nuclei from opposite mating strains (Figures 1 and 2).
Fungal nail infections are common infections of the fingernails or toenails that can cause the nail to become discolored, thick, and more likely to crack and break. The technical name for a fungal nail infection is “onychomycosis.”
Fungal nail infections can be caused by many different types of fungi (yeasts or molds) that live in the environment. Small cracks in your nail or the surrounding skin can allow these germs to enter your nail and cause an infection. Onychomycosis can be diagnosed by microscopic examination or fungal culture of the nail clipping.
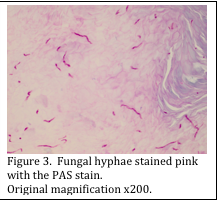
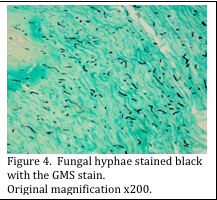
Your histology laboratory may receive skin and nail specimens to be evaluated for presence of fungi. The most common special stains used to visualize fungi are the periodic acid Schiff’s stain (PAS) and the Grocott’s methenamine stain for fungi (GMS).
Both stains are based on the chemistry of the fungal cell wall, which is made of cellulose. Cellulose is composed of glucose molecules, attached together very tightly. The PAS stain uses a primary step of oxidation of the glucose with periodic acid to form aldehyde groups.
Automate your PAS and GMS staining
New and refurbished slide stainers are available. Contact us to learn more.
Once formed, the aldehydes are available to subsequently bind with the Schiff’s reagent, which results in the fungal cell walls being stained pink (Figure 3). Diastase digestion may, or may not be used, as it does not affect the fungal staining; it simply removes any glycogen which may be present.
Some dermatopathologists feel that the GMS stain is a more sensitive stain for detection of fungi in tissue sections. In this stain, chromic acid is used to oxidize the glucose molecules, leaving the aldehyde groups open to bind silver molecules, present in the methenamine silver solution. Subsequent development and toning of the sections renders the fungal cell walls black (Figure 4).
Either the PAS or the GMS method may be utilized to stain fungi in tissue sections.
Previous blogs (Hair Histology) described how to stain fungi that are present on hair shafts.


References
- www.cdc.gov
- Scher RK, Rich P, Pariser D, Elewski B. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg. 2013 Jun;32 (2 Suppl 1):S2-4.
- http://www.microbiologybytes.com/iandi/6a.html